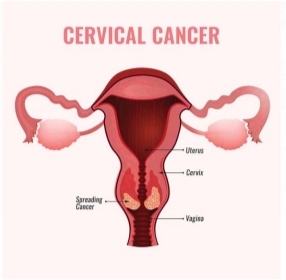
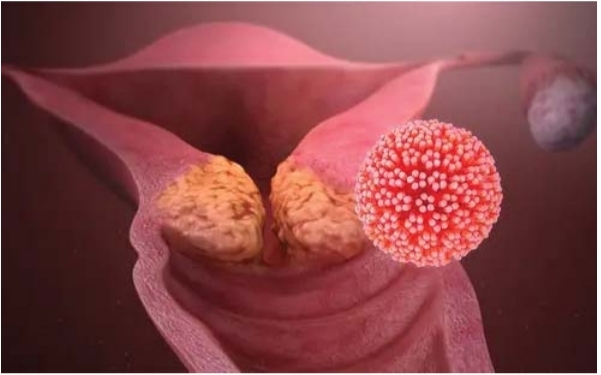
A Professor of Obstetrics and Gynaecology at the Obafemi Awolowo University Teaching Hospital Hospital, Ile-Ife, Osun State, Kayode Ajenifuja, has revealed that early detection of cervical cancer at it premalignant phase may result in almost 100% treatment success rate. He explained that during the premalignant phase, women do not experience symptoms, but that the virus can be detected through screening. Prof. Ajenifuja revealed that not less than 13 different types of Human Papillomavirus can cause cervical cancer in women and clarified that those that can cause genital warts are distinct from those that can result in cancer.
He explained that HPV16 and HPV18 are responsible for most HPV-related cancers, adding that approximately 10 per cent of women with cervix-based HPV infections will go on to have persistent HPV infections that increase their risk of developing cervical cancer. Prof. Ajenifuja further said that women contract HPV during vaginal or anal sex, adding that someone with HPV can pass the infection to another person even when they have no signs or symptoms. The Professor of Obstetrics and Gynaecology explained that cervical cancer is the second most common cancer in Nigeria and is the leading gynecology cancer in Nigeria.
He said, “The symptoms of cervical cancer include abnormal bleeding. It could be bleeding after sexual intercourse, bleeding outside the menstrual period, or post-menopausal bleeding. Other symptoms include foul-smelling virginal discharge, pain, inability to pass urinate properly, fistula, and abnormal communication between the rectum and the virginal. We don’t want women to go on and have these symptoms, which is why we advocate for early screening for the disease. “Of all the cancers, cervical cancer is the very few that we know its origin. It goes through a period of pre-cancerous phase, which can last between 15-20 years before it becomes cancer proper. “That premalignant phase is the stage we want women to screen. At that phase, women won’t have symptoms.
It’s only by screening we would know women that have the premalignant phase. “If detected at that phase, they can be treated with almost 100% success rate. But if they fail to screen at that phase, it becomes cervical cancer, and they will start having symptoms.” On how cervical cancer can be prevented, Prof. Ajenifuja said, “We have three levels of prevention. We have primary, secondary, and tertiary prevention. “However, it is more effective for girls between the ages of nine and fifteen years to get vaccinated. “When we talk about primary prevention, we don’t want an individual to have contact with the virus. How do we do that? The best form of primary prevention is vaccination. If a girl between the ages of 9-15 years is vaccinated, the virus will not be able to enter her genital tract. “But then, if we are able to vaccinate 80 per cent of girls, that means the transmission of the virus in the community will be severely limited because HVP is contracted through sexual intercourse.
Continuing, he said, “Assuming we vaccinate all the girls, there are still millions of Nigerian women with the virus who don’t know that they have it. So, that’s when secondary prevention comes in. In secondary prevention, the human already has the virus agent but doesn’t have any symptoms, and it’s through screening that the virus can be detected. “In tertiary prevention, we are just trying to limit disabilities because the woman already has the symptoms. There are two types of treatment for that – surgery or radiotherapy.” While decrying limited screening centres for cervical cancer across the country, the medical expert urged the state and local governments to provide centres in rural communities for easy access. “Screening alone does not prevent cervical cancer. We must screen and treat those detected to have the virus. “
The government is trying but we want them to do more. That 28 Nigerian women died daily of the disease is the hospital statistics. A lot of women are dying and nobody is documenting them. “So, by the time you start pulling figures from the rural communities, you will see that the figure is underrepresented. “In the rural areas, many people are dying of cervical cancer and are not being documented. So, the government should set up and step up screening centres at the LG level and at primary health centres.”
The Centres for Disease Control and Prevention described HPV as the virus that causes cervical cancer. It explained that HPV is the most common sexually transmitted disease, adding that there were about 43 million HPV infections in 2018, among many young people in their late teens and early 20s. “There are many different types of HPV. Some types can cause health problems, including genital warts and cancers. But there are vaccines that can stop these health problems from happening. HPV is a different virus than HIV and HSV (herpes). “You can get HPV by having vaginal, anal, or oral sex with someone who has the virus. It is most commonly spread during vaginal or anal sex. It also spreads through close skinto-skin touching during sex. A person with HPV can pass the infection to someone even when they have no signs or symptoms. “
If you are sexually active, you can get HPV, even if you have had sex with only one person. You also can develop symptoms years after having sex with someone who has the infection. This makes it hard to know when you first got it,” the CDC stated. According to the WHO, “Often referred to as the ‘silent killer’ and almost entirely preventable, cervical cancer is a disease of inequity of access; the new SAGE recommendation is underpinned by concerns over the slow introduction of the HPV vaccine into immunisation programmes and overall low population coverage, especially in poorer countries. “More than 95 per cent of cervical cancer is caused by sexually transmitted HPV, which is the fourth most common type of cancer in women globally with 90 per cent of these women living in low and middle-income countries.” WHO disclosed that an estimated 604,000 new cases of cervical cancer was recorded in 2020, globally. It stated that of the estimated 342,000 deaths from cervical cancer in 2020, about 90 of these occurred in low and middle-income countries.